Type a search + hit enter!

Extended breastfeeding – or nursing a child beyond the first year of life – is becoming more common in the United States due to public health efforts to normalize breastfeeding and scientific evidence of the benefits of breastfeeding. However, policy and research are only a piece of the puzzle. Social media influencers and bloggers are […]
read more
latest post

read more
Extended breastfeeding – or nursing a child beyond the first year of life – is becoming more common in the United States due to public health efforts to normalize breastfeeding and scientific evidence of the benefits of breastfeeding. However, policy and research are only a piece of the puzzle. Social media influencers and bloggers are also a huge part of the effort to normalize breastfeeding. Rachel, a mother from Michigan (@chasingthechalfants) is one of the people helping to normalize breastfeeding and has shared quite a bit of her parenting journey on Instagram. Recently, we got to interview Rachel about her experience nursing twins for 19 months. Here’s what she had to say:
Hi! My name is Rachel and I’m the face behind @chasingthechalfants on Instagram. I am a former elementary school teacher turned stay-at-home mom to a 4 year old (Landon) and 19 month old twins (Carter and Ella). My husband, 3 kids and I live in Ann Arbor, MI. When I’m not chasing after the kids, I enjoy chugging (too much) iced coffee, cooking, reading and solo trips to Target. My favorite part of being a mom is getting to be there for all the (not so) little moments and seeing their personalities develop and change. Follow along on Instagram for daily shenanigans, cooking, motherhood and more!
-
How did you fuel your body to keep up with feeding twins and has that changed over the 19 months? When the twins were born I was literally nursing around the clock and I was SO hungry. In addition to eating a variety of foods to fuel my body and theirs, I also drank a ton of water. I knew that hydration was so important and continues to be. While there were no particular foods I ate to fuel my body, I tried to eat a balanced diet but also honor any cravings I had. After all, I was feeding two little humans and was running on little sleep. As they’ve gotten older and are now nursing less, I continue to make food choices that I know will fuel me to chase after 3 toddlers. Water is still a huge piece and hydration is so important, whether you’re nursing or not.
-
What did your feeding schedule look like? I nursed on demand and continue to do so. Sometimes that means nursing one at a time and sometimes that means tandem nursing, although that’s gotten more complicated since they’ve gotten older. Thankfully a few nursing essentials made tandem nursing a lot easier – the twin Boppy pillow and the My Brest Friend Twin Pillow. Having a supportive nursing pillow to support both babies made such a huge difference.
-
When you fed at the same time, what positions did you find to work best for you? When they were younger, I always used a nursing pillow (mostly the My Brest Friend Twin pillow) or a pillow under each of them to support their heads. Now that they’re older, they’re in a whole host of positions. We joke that I am like a swim up bar – they’ll both walk up to me, have a seat and nurse! Sometimes, one will lay across my lap and the other will sit in front of me. If it sounds a little crazy, that’s because it is! But it works.
-
Did you ever worry you wouldn’t produce enough milk for both babies? Since their weights dropped significantly below birth weight after we were discharged from the hospital, we started supplementing with formula almost immediately after they were born. This actually took a lot of pressure off of me because I knew they were getting the nutrients they needed and it wasn’t solely dependent on how much milk I was producing. During the first couple months, I would nurse both babies and my husband would supplement with bottles of formula. As they got older, we have had to make a few changes due to bottle strikes, but I have always felt confident that between nursing and bottles (then formula, now whole milk), both babies were getting everything they needed.
-
What resources did you rely on when you were having a tough time breastfeeding? Outside of talking to friends and family, I mostly relied on local Facebook groups for support. We have a great local mom’s Facebook group in our city as well as local parents of multiples group. Both were great in offering support, suggestions, and being able to connect with other twin moms was especially helpful. As with most things, but especially in parenting, simply knowing that you’re not alone or not the first person to experience something is helpful in and of itself. It was also helpful to talk to friends and family who reminded me that they were there for support and that there were other breastfeeding resources available.
-
Moms say that breastfeeding adds another layer to their relationship with their infant. How did breastfeeding affect your relationship with each infant? Not surprisingly, breastfeeding twins feels a lot different than breastfeeding a singleton. In the beginning, I often felt like I was nursing 24/7 (and sometimes I actually was) so I don’t know that the breastfeeding connection was necessarily present then. But now that they’re older and things have slowed down a bit, the times when I’m able to nurse just one baby at a time is so special. As a mom, looking down and making eye contact with a nursing baby is one of the most special feelings in the world. It adds a layer of connection, love, and intimacy that I haven’t felt before. I cherish those quieter moments when I realize just how amazing my body is and what a special bond I have with each of my children.
Thank you so much, Rachel, for sharing your experience! Keep being awesome!

read more
Nutritionally, there are three monosaccharides that make up all carbohydrates: glucose, fructose, and galactose. When glucose and galactose join together, they create lactose. Lactose is the main carbohydrate present in human milk, providing ~8.5 calories per ounce of human milk. Average lactose concentrations: are stable over the first 6 months of lactation decrease slightly from […]

read more
As a nutritional biochemist, I am always interested in how we can support diet quality and food security, especially for low-income populations. Interestingly, a recent study published in the Journal of Human Lactation looked at 1,226 WIC participants found that breastfeeding duration was associated with improved diet quality for the toddler at 36 months of age. The study was a secondary analysis set up to look at within-individual associations over time. This means that rather than having any type of intervention, the researchers retrospectively analyzed data that was collected for a different study.
In order to measure the diet quality of the toddlers, the study used the USDA’s Healthy Eating Index. After conducting the phone interviews to determine the diet quality, the researchers looked back at duration of breastfeeding and found that the longer the dyad breastfed for the better the diet quality. It is important to point out that these families had nutritional support through their WIC benefits – so this speaks to the WIC program’s ability to support healthy diets for children as well.
This is not the first study to investigate the impact of breastfeeding on diet quality and similar results were found in an Australian study looking at toddler diet quality. This study found that in addition to breastfeeding status, maternal modeling of healthy eating behaviors also impacted the toddler’s diet quality.
Some studies have also looked at the interaction between breastfeeding cessation and toddler diet quality. Another study that was done in Australia found that both early breastfeeding cessation and early introduction of solids was associated with preference for energy-dense, low nutrient foods.
While we certainly don’t have a complete understanding of how children develop food preferences, we do have evidence-based recommendations that encourage children to have a healthy variety of foods in their diet:
-
Exposure: make sure your children see a variety of colors, textures, and cooking styles represented in their age-appropriate foods. Encourage your kids to put foods on their plates even if they don’t want to eat them.
-
Access: make it easy for your toddlers to access healthy foods. This can mean having appropriately sized fruits, veggies, cheese, meats, and whole grains available where they can reach them.
-
Modeling: let them see people they look up to (parents, friends, babysitters, relatives, etc.) eating foods that they may be hesitant to try.
Looking for more information about nutrition during lactation? Download my two page quick guide!

read more
On a previous edition of #milkmonday, I highlighted what the WHO Code is, why it is important, and why I, as an IBCLC, fully support the implementation of the WHO Code (amongst other supportive maternity laws and practices). But the question follows: Does the WHO Code work and can it be implemented it in such […]

read more
Medications and lactation can be a difficult topic, because there is a lot of conflicting information out there on what is safe and what should be avoided. This can be overwhelming for someone who wants to take an over-the-counter (OTC) medication to feel better but is worried about exposing his/her infant to medication. Many people end up choosing not to take anything and suffering when most medications are safe and appropriate to use during lactation.
So, how do you decide between riding it out or trying non-medication options first and taking a medication? The following points are helpful when deciding what approach to take for your symptoms and how to decrease your infant’s exposure to medications if you do need to take something for your symptoms.
-
Determine the source of your symptoms. Depending on the source of your symptoms, OTC medications may or may not be helpful. OTC medications are generally not helpful for common cold symptoms like runny nose, sore throat, and cough. These symptoms are generally caused by drainage, and the drainage is produced in response to the cold virus. The only way to reduce those symptoms is to remove the virus. Non-medication options like saline nasal rinses or hot tea with honey are helpful for clearing out drainage, making a sore throat feel better, and calming down a cough. However, OTC medications are helpful if your symptoms of runny nose, sore throat, and cough are due to seasonal allergies. In this case, the symptoms are due to the body’s response to the allergen and the release of histamine. Second generation antihistamines like Claritin, Allegra, and Zyrtec and steroid nasal sprays like Flonase will help decrease the allergic response and thus the symptoms. Regardless of the cause, Tylenol is safe for pain. Advil or Motrin (both are ibuprofen) are also safe but should be avoided if also pregnant. Colds and allergies can also cause sinus congestion. There is research to show that Sudafed, an oral nasal decongestant, can decrease milk supply. It is best to avoid Sudafed and choose a nasal spray like Afrin first.
-
Determine the likely length of time needed to treat your symptoms. If you anticipate your symptoms only lasting a few days, like with a sore back or being allergic to cats and visiting someone with cats, you should not hesitate to treat your symptoms with an appropriate medication. Cases like this usually require a couple doses of medication, and the symptoms are resolved. Any exposure via breastmilk is low and the time exposed is very short. If you anticipate your symptoms lasting for a long period of time, like with seasonal allergies, you may consider other options first. These could include avoiding your allergens, using daily sinus rinses, or choosing a nasal spray instead of an oral medication to treat your allergies. For cases like seasonal allergies, second generation antihistamines or steroid nasal sprays are safe for long-term use.
-
Try non-medication options first. Many people know that medications are safe to use when lactating but would rather try non-medication options first. This is a good choice when you feel common cold or allergy symptoms coming on or if your symptoms do not greatly interfere with daily life. Options like heating pads or ice packs are helpful for pain and inflammation. Honey is a natural cough suppressant. Warm or hot beverages like teas are soothing to sore throats. Saline nasal rinses, hot showers, and warm steam are all helpful for clearing nasal drainage and opening sinus passages. If you try non-medication options first and your symptoms worsen or you do not feel any better after a couple days, it is probably time to use a medication best suited to treat your symptoms.
-
Avoid combination medication products. It is best to take individual medications instead of combination products. The combination products often contain medication you do not need or only need for a short period of time. Taking individual medications allows you to stop medications you no longer need and thus reducing any exposure your infant may have.
-
Take short-acting medications instead of long-acting medications with the exception of antihistamines. Short-acting medications require you to take them multiple times a day instead of once or twice a day, because they do not last as long in your system. This allows you to take them only when you feel they are most needed, and it also decreases your infant’s exposure to the medication. The one exception to this general rule is antihistamines. First generation antihistamines like Benadryl are short-acting but are able to decrease milk supply when used frequently and at high doses. Second generation antihistamines are preferred since they are most specific in their actions and have not been shown to decrease milk supply even if used daily.
-
Try to take your medications after a nursing session. Many people try to take their medications immediately after a nursing session, because this provides the biggest separation between taking a medication and the next nursing session. This isn’t always possible, but it may be worth trying if you are concerned about about your infant’s exposure to a medication.
Most OTC medications are safe for short-term use, and many are safe for long-term or daily use. If you are concerned about your infant’s exposure to a medication you may take, consider what is causing your symptoms, how long you might need the medication, and what else you might be able to try first. There is no need to suffer through bothersome symptoms, and it is important to take care of yourself so you are able to take care of your family.

read more
Directly after birth we know that skin-to-skin contact had quite a few benefits for both the mother and the newborn baby. These benefits include infant temperature regulation and blood glucose control, maternal confidence in handling her infant, improved bonding between the mother and the infant, and opportunity to begin the breastfeeding relationship. With so many […]

read more
As a nutritional biochemist by training, I absolutely love when my love of nutrition collides with my love of breastfeeding. For this reason, I was so excited when I found this study that looked at maternal consumption of a low FODMAP (fermentable oligo-, di- and mono-saccharides and polyols) diet on associated infant colic symptoms.
What is a low FODMAP diet?
A low FODMAP diet aims to reduce or eliminate gas-producing foods from the diet. This reduction in gas production may help individuals who suffer from diarrhea, digestive disorders, abdominal pain, or bloating. “Gas-producing foods” are foods that contain high proportions of indigestible or poorly digested short chain carbohydrates and sugar alcohols. When foods are poorly digested, they become food for the bacteria living in your gut. When bacteria digest these carbohydrates (e.g. undergo fermentation) gas is a byproduct. Some foods that would fall into the FODMAP category include beans, lentils, wheat, and dairy.
What does this have to do with infant colic?
Colic is defined as crying for more than 3 hours per day, for 3 or more days of the week, over a span of at least 3 weeks and may show signs of gassiness. Much of the evidence that we currently have around infant colic is focused on formula fed infants. In these studies, dietary changes are made to attempt to help with colic. In an exclusively breastfed baby, infant diet (human milk) would be influenced by maternal diet. We don’t have good science looking at maternal diet changes and the associated effect on infant colic symptoms.
How did the study work?
Mothers of infants confirmed to have colic were enrolled in the study. Prior to dietary change, a milk sample and an infant fecal sample were collected. Mothers were then put on a low FODMAP diet for 7 days, and during day 5, 6, and 7, infants were reassessed for colic symptoms. On day 7 new milk and fecal samples were taken.
What did the authors find?
The trial provided a 5g/day FODMAP diet and participants in the study consumed on average 30 grams of FODMAP foods per day.
No change was found in in fecal pH or lactose content of analyzed maternal milk samples was reported.
The study did report a significant reduction in measured crying duration, crying episodes, fussing duration, combined crying-fussing times, feeding duration, and feeding episodes and a significant increase in awake-and-content duration.
What did the moms have to say?
Baby is much more content
Baby can be put down without crying
Baby’s cries are no longer pain-sounding screams
Can now read baby’s tired signs
Applying this to practice
Anecdotally, we have seen many mothers practice elimination diets and see relief in their infant’s gastrointestinal discomfort. Dairy has long been made the culprit of all infant gastro discomfort. This study shows that is may be more complex than “eliminate dairy”.
For mothers of infants with confirmed colic, a low FODMAP diet may translate to decreased infant colic symptoms.
Looking to learn more about nutrition during lactation? Download my 2 page quick guide!

read more
Early Human Development published a study this month that investigated the effect of labor medications on newborn behavior in the first hour after birth. The article caught my eye because I find myself frequently asked questions by mothers about what normal newborn behavior looks like, and quite frequently my answer is that it depends on […]

read more
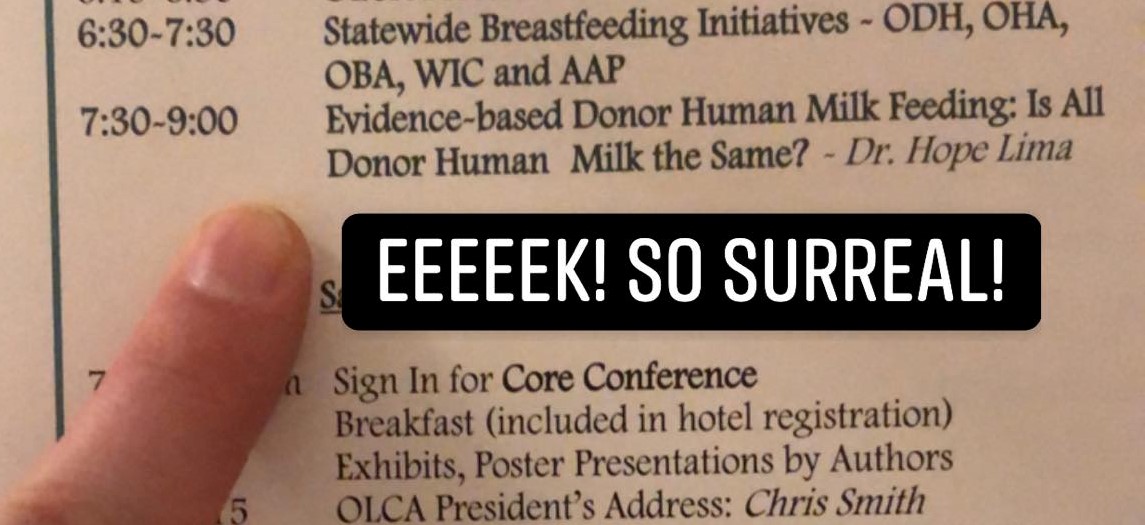
This past weekend I had the absolute honor of speaking at the Ohio Lactation Consultant Association’s annual conference: Breastfest! The experience was extremely humbling, and in addition to speaking, I got to learn from from amazing practitioners and researchers from across the country.
The conference started strong, and the first session that I attended was given by Robin Glass, author of Feeding and Swallowing Disorders in Infancy: Assessment and Management. Robin works as an OT/IBCLC at Seattle Children’s. Some new things I learned during this presentation:
- You can utilize the infant’s palmomental reflex to encourage a wide open mouth by pushing on the middle of their palm
- If you are working with an infant that has low-tone in their tongue, you can tap along the midline from the front to the back of the tongue only as far as you can see from outside the mouth
- Pulling the tongue back/up can be a compensatory strategy for weakness in the neck (when the baby pushes up with their tongue it stabilizes the neck and can help with breathing)
- When baby benefits from bilateral cheek support, you can use kinesiotaping to facilitate cheek stability
Another interesting session that I attended was given by Joni Gray, speaking on the Appalachian/American Cultural Power Code of Formula. This session was intriguing to me, as I went to school in the heart of Appalachia at West Virginia Wesleyan College. I learned quite a bit from this session. I learned that a power code is a behavior that you can engage in that makes you part of a community, and indirectly, gives you power. The context Gray put this in for breastfeeding is that in Appalachia, formula is the majority “power code” – and by choosing to breastfeed you are leaving this community for a smaller sub-community with less power. Gray’s interactive activity was the most interesting part, where we reflected on this Similac commercial:
Think about these things after you watch:
- What is the message of this commercial (overlying and underlying)?
- Does this commercial support the dominant culture of formula feeding?
- How is this commercial portraying breastfeeding moms?
- Do you feel this commercial is contributing to a cultural shift in perceptions of breastfeeding?
The last thing I am going to summarize was my experience learning from Dr. Bobby Ghaheri. The sessions led by him were extremely informative, as he specializes in infant and child tongue tie diagnosis and reversal at The Oregon Clinic. While I cannot summarize everything I learned from him here, I do have an excellent blog post he wrote & you can read it here. Tidbits I learned from Dr. Ghaheri include:
- Always assess for ties with the baby in your lap legs facing away from you and coming from above the infant
- If you are palpating below the tongue [looking for tongue tie] and there is muscle push back, you cannot be sure it is a tongue tie – you need to resolve the muscle tightness before you can determine if a tongue tie is restricting motion
- Lip tie can be recognized with blanching of lip when pulling back, nodule on the bone beneath where the lip is tied to the gums
- Anterior tongue tie is almost always hiding a posterior tongue tie
I want to wrap up this post by taking the time to thank the OLCA Breastfest Planning Committee for such an organized, professional, and intellectually stimulating weekend.

read more
Over the past 10 years we have seen a rise in the number of states where marijuana sales and use are legal. This has opened the door for women to publicly ask about, and for researchers to publicly investigate marijuana use during lactation. There are properties of marijuana that raise concern about it’s use during […]
Get Your copy →
Cross the finish line with confidence.
Don't walk into your IBCLC exam nervous - with our comprehensive study guide in your back pocket, you'll be prepared for every scenario and question.

