Type a search + hit enter!

Vitamin B6, also known as pyridoxine, is a water soluble vitamin that plays an important role as a coenzyme in the human body. A coenzyme is a molecule that binds to an enzyme allowing it to function – and pyridoxine binds to many enzymes (over 100!) that are important in energy metabolism. Good food sources […]
read more
latest post

read more
Vitamin B6, also known as pyridoxine, is a water soluble vitamin that plays an important role as a coenzyme in the human body. A coenzyme is a molecule that binds to an enzyme allowing it to function – and pyridoxine binds to many enzymes (over 100!) that are important in energy metabolism. Good food sources of pyridoxine include fish, poultry and certain nuts. Many prenatal and multivitamin/multimineral supplements contain pyridoxine. Nursing women should consume ~2 mg of vitamin B6 per day.
For a nursing mother, pyridoxine in the diet is important because concentrations in breast milk are dependent on maternal intake. A landmark study completed in 1985 showed that as maternal pyridoxine intake increased, so did concentrations in human milk. Additionally, recent research has shown that B-vitamins in human milk can fluctuate daily based on time of day, dietary intake, and when vitamin supplements are consumed – so avoiding pyridoxine is not advised.
When it comes to breastfeeding, though, nursing mothers may need to be careful about how much they are taking (particularly in supplements). According to one study, supplemental doses of pyridoxine ranging from 0.5-4.0 mg/day had no impact on serum prolactin levels or milk supply. Similarly, another study saw no impact of a maternal 100 mg intramuscular dose of pyridoxine at term. There is some evidence that high doses of B6 (600 mg/day) can cause suppression of lactation. While the body of evidence is not robust, because B6 levels in milk are easily impacted, do not advise mothers to avoid pyridoxine. It may be appropriate for an RD to evaluate B6 intake to ensure it is less than 4 mg per day if you suspect B6 intake may be impacting milk supply.
Interested in nutrition support during pregnancy or lactation? Email nutrition@hopefeedsbabies.com to set up your appointment today!

read more
Subclinical mastitis (SCM) is common, and while many IBCLCs have anecdotally recognized similarities between clients, a specific etiology is not well defined. Recent studies (1,2) have observed correlations between increased levels of proinflammatory cytokines and alterations in anti-inflammatory breast milk components and subclinical mastitis. While inflammation in and of itself is necessary for our survival, […]

read more
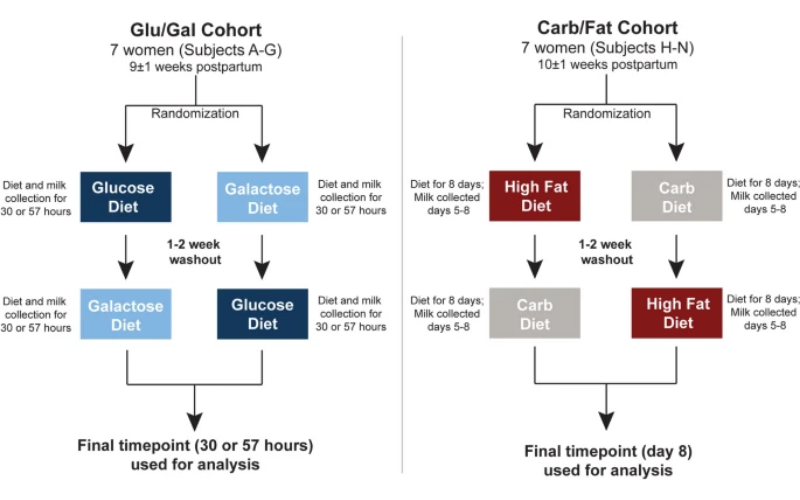
Human Milk Oligosaccharies (HMOs) are a hot topic in lactation right now. HMOs are a type of carbohydrate and many are indigestible to the infant but digestible to the bacteria that colonize the gut, facilitating growth of commensal bacteria. Additionally, HMOs may act as a decoy to pathogenic microbes, thus playing a role in infant immune protection. A recent study sought to determine if altering maternal diet could drive the HMO composition of human milk, and therefore influence the community and functional profile of the infant microbiome. The study utilized a crossover design. This study design is strong, as each participant serves as their own control. Participants were randomized into two treatment groups (Glu/Gal and Carb/Fat; see below figure). The researchers defined the carb diet as consuming 60% of calories from carbohydrates and a high fat diet as consuming 55% of calories from fat. Note: 60% of calories from carbohydrates is considered by most nutrition professionals as a healthy carbohydrate intake.
General Findings
-
The Gal diet significantly increased the total concentration of HMO-bound fucose and proportionately increased the inferred abundance of fucosidase (an enzyme expressed by bacteria in the microbiome)
-
A high fat diet (55% of calories) diet significantly reduced the total concentration of HMO-bound sialic acid when compared to a high carbohydrate (60% of calories) diet
-
The Gal diet and the high fat diet both increased concentrations of HMOs in individual participants when compared to their baseline
-
Diet did not impact any subject’s individual taxonomic composition of the milk microbiome (e.g. population make up)
-
Diet did alter which metabolic pathways were active in the human milk microbiome and to what extent they were activated
-
These metabolic changes are unlikely to have any clinical impact on the infant, as the quantity of substrates (e.g. proteins, carbohydrates) being synthesized is still very low in comparison to substrates of maternal origin
-
-
Certain fucosylated HMOs confer a growth advantage to Streptococcus spp. expressing the fucosidase enzyme
Authors speculate the growth advantage of the Streptococcus spp., encouraged by fucosylated HMOs may help with prevention of mastitis in the parent and promote Streptococcus proliferation in the infant GI tract. The authors original hypothesis seems to be supported – altering maternal diet can drive the HMO composition of human milk.
The changes the authors observe in this article support the current dietary recommendations of 45-65% of calories coming from carbohydrates and 20-35% of calories coming from fat. This is drawn from the data showing that HMO-bound sialic acid is increased when dietary carbohydrates make up 60% of daily calories. Additionally, this data suggests that inclusion of galactose as a carbohydrate source may play a role in the level of HMO-bound fucose, potentially interacting with and providing a growth advantage to Streptococcus spp bacteria. Galactose is a monosaccharide (single sugar molecule) that is found in dairy products and has a lower glycemic index than glucose (25 as compared to 100, respectively).
Existing literature suggests that a maternal high-fat diet is associated with gut microbiome changes in the infant (1). These changes may be associated with negative, long-term health outcomes in the infant, such as asthma and type 1 diabetes (2,3).
As a dietitian, I do not recommend high-fat (ketogenic) diets (or any diets for that matter), as any weight that is lost is likely to be regained unless a true dietary lifestyle (e.g. not restrictive) change occurs.

read more
Oh caffeine… whether it is the coffees, sodas, teas or the like, many of us are addicted to caffeine. However, when you are pregnant and/or breastfeeding your caffeine habits may need to change. So, what is caffeine? Although many refer to caffeine as energy, caffeine does not provide your body with energy. Scientifically, energy for […]

read more
Did you know that postpartum nutrition looks different than nutrition before and during pregnancy? Hunger can skyrocket if you are breastfeeding, and food restrictions loosen up (allowing incorporation of ALL those foods you missed!). This can be challenging for some, especially if there is a goal to lose weight after delivering. However, it is vital to properly fuel your body especially if you are breastfeeding. This means feeling confident in meeting all of your nutrient requirements WITHOUT feeling hungry or restricted. That is why Rebekah Culp, MS, RDN, LD has created the Comprehensive Lactation + Postpartum Nutrition Guide. In this resource you will find information on how to build a healthy plate, the best way to lose weight, key nutrients for lactation, general food safety and more! Most importantly, all of the content is tailored to postpartum and lactation needs – so you can get information that is applicable to your specific life stage.
Check out the parent resources for more information. If you are interested in a more tailored, one-on-one approach to your postpartum nutrition, you can schedule a nutrition consult with one of our Registered Dietitians today to help you reach your goals by emailing nutrition@hopefeedsbabies.com.

read more
Cannabinoids are a class of naturally occurring, biologically active molecules. Delta-9-tetrahydrocannabinol, more commonly known as THC, is a psychoactive cannabinoid found in marijuana – this is not produced in the human body. There are cannabinoids produced by the human body (endogenous cannabinoids) that act on the endocannabinoid system (ECS) to elicit neurological responses by binding […]

read more
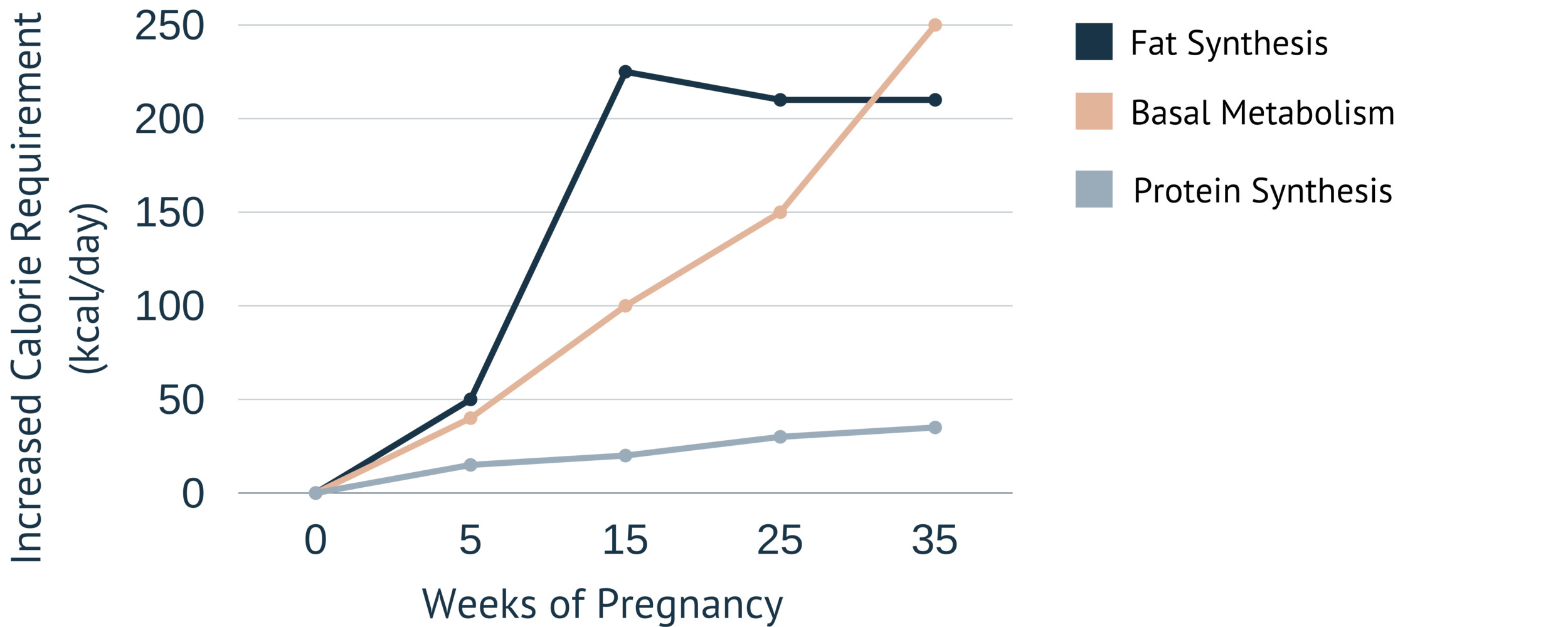
Increased hunger is a natural occurrence during pregnancy, as there is a tiny human growing. However, those energy (calorie) requirements are not of a second full-grown human. So, how much do energy requirements change during pregnancy? Let’s have a look:
As you can see in the above image, the further along in pregnancy, the higher the energy needs are. A majority of the extra calories consumed during pregnancy are used for fat synthesis. Fat synthesis is important during pregnancy, as these fat stores will be mobilized during the postpartum period to ensure adequate milk fat concentrations for the newborn. The extra calories also support tissue generation through protein synthesis in the placenta and uterus.
The weight gain guidelines from the Institute of Medicine range from 11 to 40 pounds throughout pregnancy. It is also the recommendation of the Institute of Medicine that most of that weight be gained in the second and third trimesters of pregnancy. Despite these (seemingly) specific numbers, energy needs vary from woman to woman. I always recommend that women listen to their body. Eat when feeling hungry, choosing foods high in nutrients. Drink when feeling thirsty. And remember, women know their bodies. It is our job as practitioners to remind them that they do.
Are you looking for more individualized support? Can now meet virtually with a Registered Dietitian through Hope Feeds Babies. Click below to schedule!

read more
Extended breastfeeding – or nursing a child beyond the first year of life – is becoming more common in the United States due to public health efforts to normalize breastfeeding and scientific evidence of the benefits of breastfeeding. However, policy and research are only a piece of the puzzle. Social media influencers and bloggers are […]

read more
Nutritionally, there are three monosaccharides that make up all carbohydrates: glucose, fructose, and galactose. When glucose and galactose join together, they create lactose. Lactose is the main carbohydrate present in human milk, providing ~8.5 calories per ounce of human milk. Average lactose concentrations:
-
are stable over the first 6 months of lactation
-
decrease slightly from 6 months-1 year and then remain stable over the second year of lactation
-
are higher if the infant is feeding frequently and lower if it has been a while since the infant has fed
Lactose is an interesting disaccharide, because infants are able to digest it due to the release of an enzyme called lactase. Lactase breaks the bond between glucose and galactose, both of which can be absorbed into the body. From birth, infants with galactosemia cannot consume lactose – not from breast milk or standard infant formula. Galactosemia is an inability to produce energy from galactose, and so levels in the blood rise. This can have severe consequences, including failure to thrive and death if not diagnosed.
Human milk oligosaccharides (HMOs) are also carbohydrates, but they do not provide any caloric value to the infant. HMOs serve as a food source for beneficial bacteria and can also have a direct impact on the infant’s immune response.
From what we know about HMOs:
-
there are over 200 structures
-
mothers secrete a consistent profile of HMOs
-
different mothers secrete different types of HMOs
Human milk oligosaccharides can also be protective of viral and bacterial causes of diarrhea – depending on secretor status and Lewis antigen status of the HMOs produced.
Glycoconjugates are carbohydrates bound to protein or lipid molecules. These molecules are important for the infants innate immune response. A well known example of a glycoconjugate is lactoferrin – a molecule that serves as a bacteriocide and fungicide by hydrolyzing their RNA. Lactoferrin also serves as a stimulant to small intestine maturation in the newborn. Interestingly, lactoferrin has also been implicated in bone health in postmenopausal women, and more recent research is looking at the impact of lactoferrin on healthy infants.
The more I learn, the more I am convinced: human milk is magic.
Looking for more information about nutrition and lactation? Click below to download my 2 page resource on tips!

read more
As a nutritional biochemist, I am always interested in how we can support diet quality and food security, especially for low-income populations. Interestingly, a recent study published in the Journal of Human Lactation looked at 1,226 WIC participants found that breastfeeding duration was associated with improved diet quality for the toddler at 36 months of […]
Get Your copy →
Cross the finish line with confidence.
Don't walk into your IBCLC exam nervous - with our comprehensive study guide in your back pocket, you'll be prepared for every scenario and question.